Copays take effect for immigrant health programs as cost estimates continue to decline
By JERRY NOWICKI
Capitol News Illinois
[email protected]
Cost estimates for a pair of state-funded health care programs serving certain low-income noncitizens have declined by tens of millions of dollars in recent months as the state rolled out new copay and co-insurance requirements this week.
The Health Benefits for Immigrant Adults and Health Benefits for Immigrant Seniors programs provide state-funded Medicaid-like benefits to individuals aged 42 and over who would otherwise be eligible for the federal low-income health care program if not for their immigration status.
That includes those in the U.S. without legal permission and those who have obtained a green card but not yet completed a five-year waiting period to earn federal benefits. Individuals who have applied for asylum or sanctuary in the U.S. – which includes many of the more than 34,000 migrants bused to Illinois from Texas in the last year-and-a-half – more likely qualify for other preexisting state or federal benefits.
Advocates for the programs contend they are not only lifesaving but also cost-saving in the long-run as they give individuals access to preventative care rather than making them reliant upon expensive emergency room visits to treat conditions that worsen due to lack of care. Opponents of the programs, namely Republican lawmakers, have criticized them as an expensive enticement for people illegally residing in the U.S. to relocate to Illinois.
The programs, originally launched for those aged 65 and older in 2020 then expanded in waves, became a sticking point in state budget negotiations last year when Gov. JB Pritzker’s administration projected their single-year costs to exceed $1 billion.
But current estimates now project the programs will cost $773 million in the current fiscal year. Those estimates, however, have declined by $60 million since August, the month following the Pritzker administration’s initial announcement of certain cost-saving measures.
Read more: Pritzker quickly wields expanded authority to freeze noncitizen health care enrollment
Cost-saving measures
Ultimately, the contentious budget negotiations ended last year with lawmakers allocating $500 million in funding to the program from the state’s General Revenue Fund and giving the Pritzker administration authority to limit program enrollment and costs.
The administration in turn paused enrollment in HBIA as of July 1 and in HBIS as of Nov. 6. The two programs now collectively serve about 69,000 people aged 42 and older, and enrollment remains paused.
In January, the administration also began moving enrollees to the state’s Medicaid managed care program, which connects individuals with private insurers who contract with the state to oversee routine and follow-up health care.
The Department of Healthcare and Family Services, which administers the programs, expects the managed care transition to be complete in April.
After months of delays, the department announced that copays and co-insurance for certain services went live Thursday.
“Most services covered by the HBIA and HBIS programs … will continue to be free for customers, including primary care visits, prescription medications and vaccinations at a pharmacy or doctor’s office,” the department said in a news release. “The new copays and co-insurance will apply to the use of non-emergency hospital or surgical center services, like nonemergent elective surgeries, physical therapy and lab work.”
Enrollees may see a $250 copay per nonemergency inpatient hospitalization and a 10 percent charge for nonemergency outpatient services or care received from ambulatory surgical treatment centers. It’s a major difference from the federally funded Medicaid program, which does not require copays.
Whether individuals are subject to those copays and co-insurance requirements will depend on if they have already been enrolled in managed care and which managed care organization is serving them, according to the department. The state reimburses managed care organizations at a specified rate, giving the MCOs authority to charge copays or co-insurance without requiring them to do so.
CountyCare in Cook County, where most program enrollees are located, is waiving all copays and coinsurance requirements, per the department.
The department announced it no longer plans to issue a copay for emergency room visits.
The Healthy Illinois Campaign, a statewide coalition of immigrant and health care advocates, has pushed for an expansion of the program and fought any efforts to limit it or install cost-sharing.
The group’s director, Tovia Siegel, praised the administration’s decision not to charge a copay for emergency room care but said the other copays “place a significant burden on both providers and patients, limiting access to healthcare for Illinois’ immigrant community.”
The copays, advocates noted, are charged to medical providers by MCOs, but the providers are required to collect them from patients, creating an administrative burden. As well, they warned that individuals may choose to defer certain “elective” procedures, such as a colonoscopy, due to the copay requirement, potentially undermining the program’s preventative care goals.
“We urge the Department of Healthcare and Family Services and Managed Care Organizations to reconsider implementing these charges, which will generate a relatively small amount of money but can be the difference between life and death for low-income Illinoisans,” Siegel said in a statement.
Costs declining
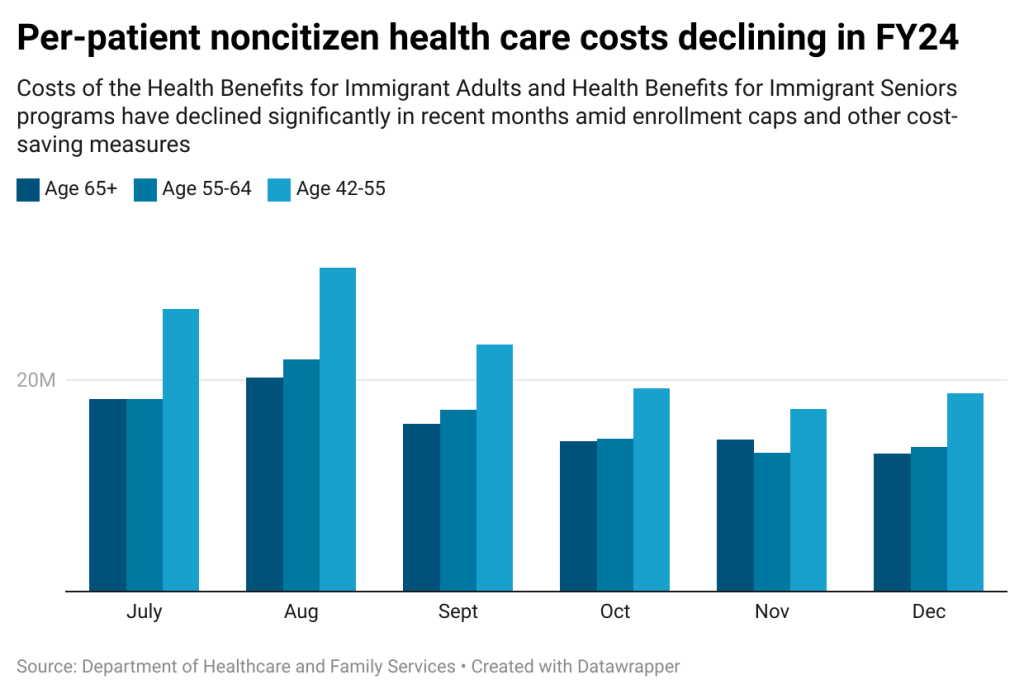
The programs’ cost estimates, meanwhile, have been on the decline amid the administration’s savings measures. In September, an HFS analysis estimated the programs’ 12-month cost to be $832 million for the fiscal year that ends June 30. But the department’s latest estimate, published Jan. 9, now projects the programs will cost $773 million. In total, the state has spent nearly $330 million collectively on the programs in the first six months of the fiscal year, per the January estimate.
The department’s data shows average monthly costs for the programs decreased steadily between August and December, from $72.7 million to $45.3 million.
When the state announced its enrollment caps, it noted per-enrollee costs were higher among the HBIA and HBIS populations “due to more prevalent, untreated chronic conditions and higher hospital costs.” With the caps in place, the program is now populated with individuals who’ve been receiving routine care, rather than a steady stream of new enrollees who are more expensive to insure.
Thus, the per-patient monthly costs have also declined. In August, per-patient costs reached $1,232 for enrolled individuals aged 65 and older, $1,295 for those aged 55-64, and $844 for those aged 42-54. In December, those numbers declined to $778, $805 and $541, respectively.
Advocates pointed to those declines as evidence that the programs are accomplishing their intended goal of replacing costly emergency care with more cost-efficient preventative services.
“While there are several potential explanations, cost decreases in the HBIA and HBIS programs can be an indication that enrollees are receiving more preventative care and therefore needing less intensive, expensive care,” Siegel said. “However, the implementation of copays could threaten these gains as enrollees are dissuaded from receiving this cost-saving preventative care.”
Capitol News Illinois is a nonprofit, nonpartisan news service covering state government. It is distributed to hundreds of newspapers, radio and TV stations statewide. It is funded primarily by the Illinois Press Foundation and the Robert R. McCormick Foundation, along with major contributions from the Illinois Broadcasters Foundation and Southern Illinois Editorial Association.